Unique Challenges to Heparin Monitoring in Neonatal and Pediatric Populations
A Need for a Near-Patient Rapid Heparin Monitoring Test That Utilizes Low Sample Volume
Each year, around 40,000 newborns are diagnosed with congenital heart defects1 and some of them may require surgery and eventual anticoagulation monitoring. Other scenarios for anticoagulation monitoring include those in pediatric intensive care (PICU) or receiving extracorporeal membrane oxygenation (ECMO). Over the past decade, there has been a dramatic increase in the use of anticoagulation therapies in pediatric patients, with up to 15% of hospitalized children receiving heparin or heparinoids2,3,4.
One of the major challenges of anticoagulation therapy in neonates and children is the narrow therapeutic window of various anticoagulants. Additionally, many anticoagulants have complex pharmacodynamic and pharmacokinetic properties that lead to significant variation in anticoagulant response among children, even at the same weight-adjusted dose5. The variation in response is especially pronounced in neonates due to an immature hemostatic system6. This can lead to frequent monitoring (2-3 times per day) to ensure appropriate anticoagulation7.
High-volume Blood Draws Present Significant Risks to Small Children
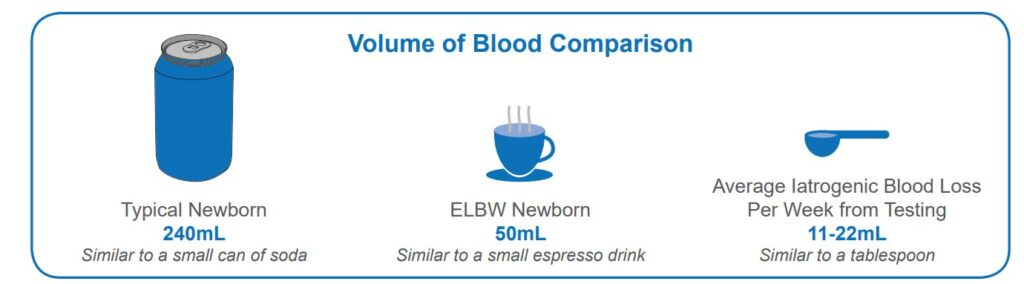
In a PICU setting, clinicians require a multitude of lab tests, each requiring a significant volume of blood (Fig. 1). Activated Partial Thromboplastin clotting time (aPTT), anti-Factor Xa activity (afXa) and/or anti-thrombin function (ATIII) tests are typically used to monitor heparin therapy. These tests require blood samples of as much as ~2-3 mL from pediatric patients. One study in preterm infants found that on average, roughly one-third of their total blood volume was lost to laboratory tests in their first month of life.8. Frequent blood collection from low-weight patients can cause anemia and may require blood transfusions, which in turn can result in infections, antibiotic therapies, and longer hospital stays.
Fig. 1. Volume of blood in a typical newborn, extremely low birth weight (ELBW) newborn and average volume of blood loss per week during the first 6 weeks of life, portrayed as everyday objects for scale comparison.
Extended Test Turnaround Time Limits Timely Clinical Decision-Making
Near-Patient Testing for Monitoring Heparin Therapy
Digital microfluidics (DMF) technology is best suited to maximize diagnostic yield by rapidly performing different types of tests near-patient using low sample volume . Feasibility testing of a DMF afXa test with a ~ 50 µL whole blood input and ~14 minutes time-to-result was performed in collaboration with Children’s Hospital of Atlanta (For Research Use Only. Not for use in Diagnostic Procedures). Data obtained on the DMF platform correlated well with an FDA-approved comparator (poster presented at 2023 ADLM Annual meeting at Anaheim). Further testing of this assay across multiple sites is in progress.
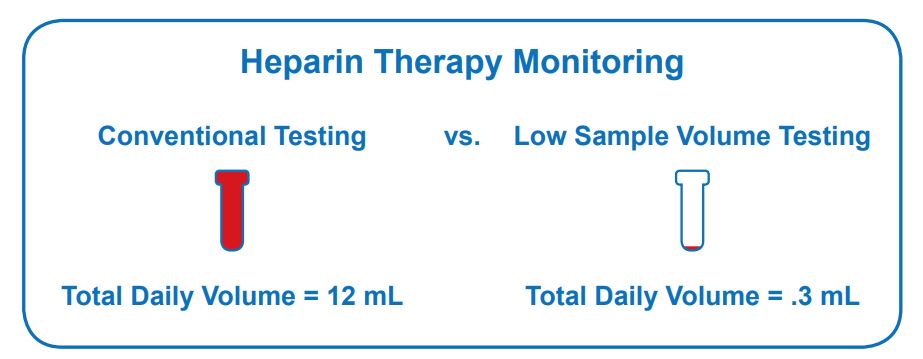
Fig. 2. Comparison of daily volume of blood taken in conventional testing and low sample volume testing, for combination of tests used in standard heparin therapy monitoring.
A rapid afXa test that can be performed near–patient and utilizes low blood volume would be a key benefit to neonatal and pediatric patients who are susceptible to anemia due to recurrent lab testing (Fig 2).
**Test is not available for sale or use in any territory at this time.
References
- https://www.cdc.gov/ncbddd/heartdefects/data.html
- Francis JL, Groce JB, 3rd and Heparin Consensus G. Challenges in variation and responsiveness of unfractionated heparin. Pharmacotherapy. 2004;24:108S-119S.
- Newall F, Barnes C, Ignjatovic V and Monagle P. Heparin-induced thrombocytopenia in children. J Paediatr Child Health. 2003;39:289-92.
- Raffini L, Huang YS, Witmer C and Feudtner C. Dramatic increase in venous thromboembolism in children’s hospitals in the United States from 2001 to 2007. Pediatrics. 2009;124:1001-8.
- Hirsh J, Anand SS, Halperin JL, Fuster V and American Heart A. AHA Scientific Statement: Guide to anticoagulant therapy: heparin: a statement for healthcare professionals from the American Heart Association. Arterioscler Thromb Vasc Biol. 2001;21:E9-9.
- Andrew M, Vegh P, Johnston M, Bowker J, Ofosu F and Mitchell L. Maturation of the hemostatic system during childhood. Blood. 1992;80:1998-2005.
- McCrindle BW, Li JS, Manlhiot C, Tweddell JS, Giglia TM, Massicotte MP, Monagle P, Krishnamurthy R, Mahaffey KW, Michelson AD, Verdun N, Almond CS, Newburger JW, Brandao LR, Esmon CT, Manco-Johnson MJ, Ichord R, Ortel TL, Chan AK, Portman R, Rose M, Strony J and Kaltman JR. Challenges and priorities for research: a report from the National Heart, Lung, and Blood Institute (NHLBI)/National Institutes of Health (NIH) Working Group on thrombosis in pediatric cardiology and congenital heart disease. Circulation. 2014;130:1192-203.
- Counsilman, Clare E., et al. “Iatrogenic blood loss in extreme preterm infants due to frequent laboratory tests and procedures.” The Journal of Maternal-Fetal & Neonatal Medicine 34.16 (2021): 2660-2665.